Amoebiasis
20-Point Summary Table: Amoebiasis
| 🔢 No. | 🧠 Topic | 📌 Key Point |
|---|---|---|
| 1️⃣ | Definition | Amoebiasis is an intestinal infection caused by Entamoeba histolytica. |
| 2️⃣ | Causative Agent | Entamoeba histolytica, a pathogenic protozoan amoeba. |
| 3️⃣ | Reservoir | Infected humans (asymptomatic cyst passers and patients). |
| 4️⃣ | Mode of Transmission | Feco-oral route via contaminated food/water or hands. |
| 5️⃣ | Infective Form | Mature quadrinucleate cyst of E. histolytica. |
| 6️⃣ | Site of Infection | Primarily the colon (cecum, ascending colon, rectum). |
| 7️⃣ | Trophozoite Features | Motile, with single nucleus, ingests RBCs (pathognomonic). |
| 8️⃣ | Cyst Features | Non-motile, 1–4 nuclei, infective in nature. |
| 9️⃣ | Asymptomatic Carrier | Can transmit infection via cysts in stool. |
| 🔟 | Intestinal Amoebiasis | Presents as diarrhea, abdominal pain, and dysentery. |
| 1️⃣1️⃣ | Amoebic Dysentery | Bloody mucoid stools, tenesmus, cramping — no fever usually. |
| 1️⃣2️⃣ | Extraintestinal Disease | Amoebic liver abscess is the most common complication. |
| 1️⃣3️⃣ | Liver Abscess Features | Right lobe > left, tender hepatomegaly, “anchovy sauce” pus. |
| 1️⃣4️⃣ | Diagnosis (Stool) | Microscopy shows trophozoites with ingested RBCs. |
| 1️⃣5️⃣ | Diagnosis (Serology) | Anti-amoebic antibody tests (useful in liver abscess). |
| 1️⃣6️⃣ | Imaging (Liver Abscess) | Ultrasound or CT reveals hypoechoic lesion in liver. |
| 1️⃣7️⃣ | Medical Treatment | Metronidazole + luminal agent (diloxanide furoate). |
| 1️⃣8️⃣ | Surgical Indications | Rare — done for rupture of abscess into peritoneum. |
| 1️⃣9️⃣ | Prevention | Safe water, hand hygiene, sanitation, avoid raw salads. |
| 2️⃣0️⃣ | Important Differentials | Bacillary dysentery, IBD, other parasitic infections. |
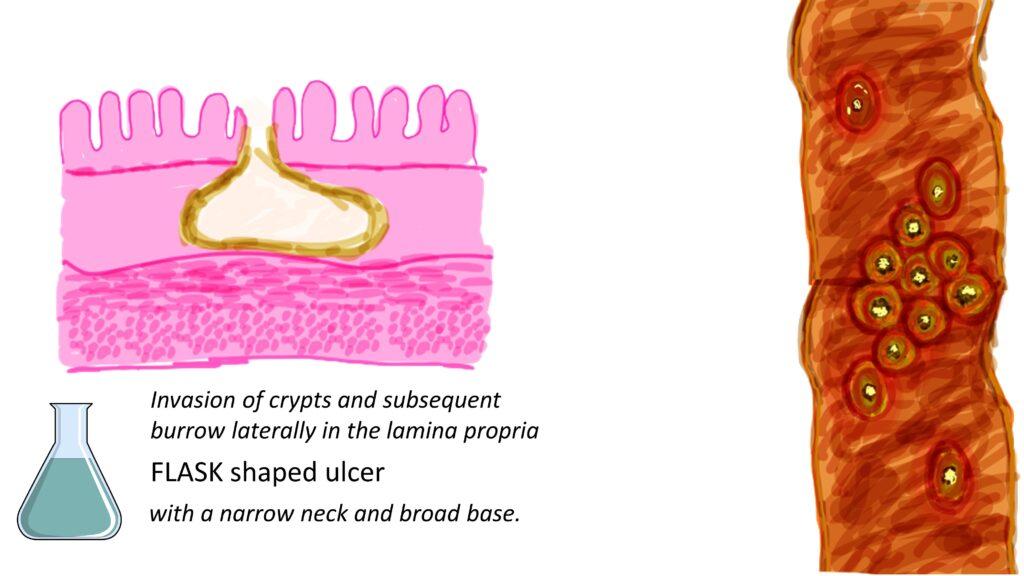
Flask-shaped ulcers are a characteristic pathological feature of invasive amoebiasis, particularly amoebic colitis, caused by the parasite Entamoeba histolytica.
Here’s a breakdown of how they form and their significance:
Formation
- Invasion: Pathogenic E. histolytica trophozoites, released from cysts in the intestines, invade the crypts of the colonic glands and burrow into the submucosa.
- Lateral Extension: The invasion is typically halted by the muscularis propria, causing the trophozoites to spread laterally within the submucosa.
- Inflammation and Necrosis: This lateral burrowing and the host’s inflammatory response lead to necrosis and the development of the characteristic flask-shaped ulcer.
- Undermining the Mucosa: The base of the ulcer is broader than the apex, undermining the overlying mucosa.
Key features
- Shape: Resembles a flask or bottle with a narrow neck and a broader base.
- Location: Commonly found in the cecum and ascending colon, but can occur anywhere in the colon.
- Histology: Trophozoites are often seen at the base of the ulcer and within the submucosa, along with necrotic debris and inflammatory cells.
Significance in diagnosis
- The presence of flask-shaped ulcers on colonoscopy and/or biopsy is highly suggestive of amoebic colitis.
- However, it’s important to note that other conditions like Balantidium coli (Balantioides coli) infection can also cause similar ulcers.
- Therefore, definitive diagnosis relies on identifying E. histolytica trophozoites in tissue biopsies, stool samples, or through molecular tests like PCR.
Differentiation from other conditions
- Amoebic colitis can sometimes resemble other conditions like inflammatory bowel disease (IBD).
- Features that can help differentiate amoebiasis from IBD include:
- Discrete ulcers with intervening normal mucosa in amoebiasis, while IBD often presents with continuous inflammation.
- The presence of necrotic material and trophozoites lining the ulcers in amoebiasis.
- Specific identification of E. histolytica through appropriate testing.
In conclusion, the flask-shaped ulcer is a distinctive feature of invasive amoebiasis, offering crucial clues for diagnosis when observed through endoscopic examination and confirmed by histopathological analysis or specific laboratory tests.
**Amoebiasis** is caused by trophozoite invasion and necrosis, typically seen in the large intestine on biopsy. This helps differentiate it from bacterial ulcers. Amoebiasis results from trophozoite invasion and necrosis in the large intestine on biopsy. This helps distinguish it from bacterial ulcers. The flask-shaped ulcers are a characteristic feature of invasive amoebiasis caused by Entamoeba histolytica. They offer essential clues for diagnosis during endoscopic examination. Confirmation is done through histopathological analysis or specific laboratory tests.